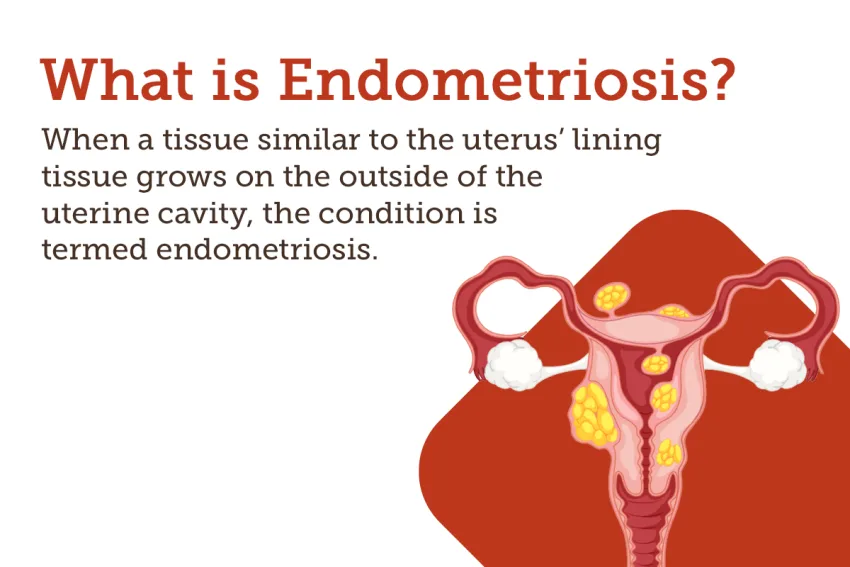
Endometriosis is a chronic and often debilitating condition that affects millions of women around the world. It occurs when tissue similar to the lining of the uterus grows outside of it, causing pain, infertility, and other symptoms. Despite its prevalence, endometriosis remains poorly understood by many healthcare professionals and patients alike.
The impact of endometriosis on women’s lives cannot be overstated. For some, it means missing work or school due to excruciating menstrual cramps; for others, it can mean undergoing multiple surgeries in an attempt to manage their symptoms. Yet despite the significant toll this condition takes on individuals and society as a whole, there has been relatively little progress made in terms of treatment options or even basic research into its underlying causes.
This article seeks to shed light on this complex and under recognized condition by exploring recent advances in our understanding of endometriosis. From promising new diagnostic tools to emerging treatments that target the root cause of the disease rather than just managing its symptoms, there is a reason for the hope that we may soon see real progress in improving outcomes for those living with endometriosis.
Understanding Endometriosis
So, you’ve heard of endometriosis? Congratulations on being ahead of the curve! Do you know what’s truly innovative? Understanding a medical condition that affects 1 in 10 women. That’s right – millions of people are affected by this condition and yet so many still don’t understand what it is or how to treat it.
Let’s start at square one: What is endometriosis? Essentially, it’s when the lining of your uterus (the endometrium) grows outside of your uterus instead of shedding during menstruation. This can cause all kinds of problems like pain, infertility, and even bowel issues. It sounds pretty unpleasant, doesn’t it?
Unfortunately, there isn’t just one straightforward treatment for endometriosis. Some people opt for surgery while others try hormone therapy or pain relief medication. It depends on the severity of their symptoms and personal preference. The good news is that with proper management and care from healthcare professionals, those who suffer from endometriosis can lead fulfilling lives without letting their condition hold them back.
Now that we’ve covered the basics, let’s dive into some specifics about the symptoms of endometriosis. But first, take a moment to appreciate yourself for wanting to learn more about this under-discussed topic – knowledge is power after all.
Symptoms Of Endometriosis
Have you ever felt like your uterus is a ticking time bomb? Endometriosis can make it feel that way. This condition affects up to 10% of women in their reproductive years and is characterized by the growth of tissue similar to the lining of the uterus outside of it.
The symptoms of endometriosis vary from person to person, but some common signs include painful periods, pain during sex or bowel movements, heavy bleeding, fatigue, and infertility. It’s important to note that not everyone with endometriosis experiences all of these symptoms, and some people may have no symptoms at all.
If you suspect you may have endometriosis, it’s essential to seek medical attention for an accurate diagnosis. Your doctor will likely perform a pelvic exam and order imaging tests such as an ultrasound or MRI. In severe cases, surgery may be necessary for both diagnosis and treatment. There are also medications available to manage symptoms and slow down the progression of the disease depending on its stage.
Understanding the symptoms of endometriosis is just one step toward managing this condition effectively. In our next section, we’ll explore what causes this condition so we can take another step forward in finding innovative solutions for those who suffer from it.
Causes Of Endometriosis
Have you ever wondered about the causes of endometriosis? It’s a common condition that affects one in ten women worldwide. Endometriosis is when tissue similar to the lining of your uterus grows outside the womb, causing severe pain and infertility. While there are many theories on what causes this disease, researchers have yet to determine its exact origins.
There seem to be several factors that may contribute to the development of endometriosis. Genetics plays a role since it tends to run in families. Hormones also appear to play a part as estrogen is known to promote growth in these abnormal tissues. Additionally, immune system dysfunction could allow endometrial cells from menstruation to travel through the bloodstream and attach themselves elsewhere in the body.
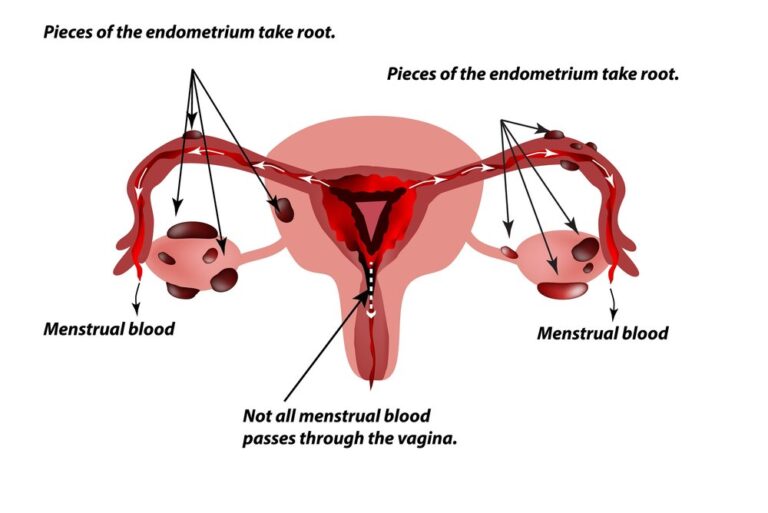
Endometriosis surgery is another potential cause for developing this condition. Studies show that surgical procedures involving the reproductive organs can increase the risk of endometrial implants forming at places like incision sites or scar tissue. Furthermore, some experts believe that menstrual blood flowing backward into the fallopian tubes during periods (called retrograde menstruation) could be responsible for seeding new areas with endometrial cells. Overall, more research needs to be done before we can definitively say what causes endometriosis. but understanding these possible risk factors is an important starting point for tackling this debilitating disease head-on.
Diagnosis Of Endometriosis
If you’re experiencing painful periods, pelvic pain, or infertility issues, your doctor may suspect endometriosis. But how is this condition diagnosed? Endometriosis can be challenging to diagnose because its symptoms are similar to many other health problems. However, proper diagnosis is crucial for successful treatment and symptom management.
To diagnose endometriosis, the first step typically involves a physical exam with your gynecologist. During this examination, the doctor will feel for any signs of abnormal growths or cysts in the pelvic area that could indicate endometriosis. They may also perform an ultrasound or MRI scan to capture images of your reproductive organs and look for potential abnormalities.
In some cases, laparoscopy may be necessary to confirm a diagnosis of endometriosis definitively. This minimally invasive surgical procedure allows doctors to view the pelvis through small incisions made near the navel. The surgeon will examine your reproductive organs directly and take tissue samples if needed for further testing. With modern technology advancements such as AI integration into medical procedures, there’s no telling what new diagnostic methods we might see in diagnosing conditions like endometriosis in the future.
As more research emerges about endometriosis, including its causes and risk factors, so too does our understanding of effective ways to diagnose it early on before symptoms worsen over time. If you experience any unusual menstrual symptoms or ongoing pelvic pain that doesn’t subside after taking over-the-counter medications like ibuprofen or acetaminophen, don’t hesitate to speak with your healthcare provider about possible next steps toward getting an accurate diagnosis and appropriate treatment plan in place. In the following section let’s delve deeper into various stages of endometriosis.
Stages Of Endometriosis
Endometriosis is a condition that affects millions of women worldwide. Though it can be challenging to diagnose, understanding the stages of endometriosis can help patients better understand their symptoms and treatment options.
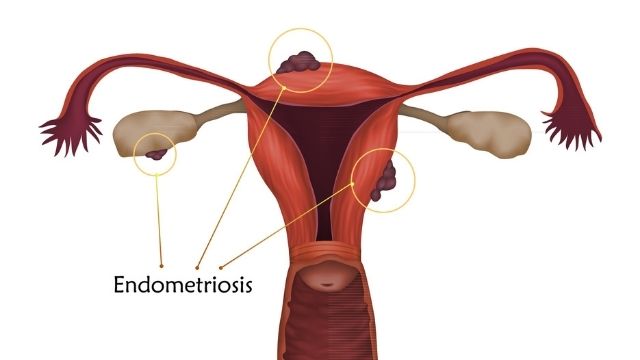
At stage one, endometrial tissue may be present outside of the uterus but is limited in size and scope. At this stage, patients may experience mild pain or discomfort during menstruation or intercourse. As the disease progresses into stages two and three, the implants grow larger and deeper into surrounding tissues. Painful periods become more severe, sometimes accompanied by nausea and fatigue. In some cases, cysts called endo-metriomas may develop on the ovaries, causing painful swelling and scarring.
Finally, at stage four the most severe form of endometriosis the growths have spread throughout multiple organs within the body. Patients often describe intense pelvic pain even when not on their period. The adhesions resulting from advanced-stage endometriosis can cause infertility if left untreated for too long.
Understanding these different stages underscores how important early diagnosis and management are for treating endometriosis effectively. With appropriate medical care, many women with this condition go on to lead healthy lives without debilitating pain or fertility issues.
As we delve further into exploring treatment options for endometriosis, it’s essential to keep these different stages in mind as they dictate which treatments will work best for each patient’s unique situation.
Treatment Options For Endometriosis
When it comes to treating endometriosis, there are various options available. It’s important to note that the treatment plan will depend on the severity of the condition and how much pain you’re experiencing. Some women may find relief through medication, while others might require more invasive procedures.
One idiom that perfectly sums up the situation is ‘different strokes for different folks’. This phrase emphasizes that everyone’s experience with endometriosis is unique and requires personalized care. For instance, hormone therapy can help manage symptoms like heavy bleeding or painful menstrual cramps. However, if this approach doesn’t work for you, surgery could be a better option.
Surgeries for endometriosis usually involve removing tissue growths, cysts, or scar tissues from inside your body. Laparoscopic surgeries are minimally invasive procedures where doctors make small incisions in your abdomen and use special instruments to remove the affected tissues. In severe cases where other treatments have failed, a hysterectomy (removal of the uterus) might be necessary to alleviate chronic pain.
In summary, finding an effective treatment strategy for endometriosis involves working closely with your doctor and experimenting with different approaches until something works best for you. The next section will delve deeper into how women manage the pain associated with endometriosis – another crucial aspect of living with this condition.
Pain Management For Endometriosis
Dealing with the excruciating pain that comes with endometriosis can be a never-ending struggle for many women. While there are various treatment options available, finding effective pain management techniques is crucial to cope with this condition. However, some people might argue that managing the pain alone cannot solve the problem in its entirety. But let’s admit it; not everyone has access to all possible treatments or wants to take an aggressive approach toward their health.
One of the most widely recommended strategies for managing endometriosis pain is through medication. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen sodium have shown promising results in reducing period cramps and pelvic discomfort. Women who experience severe menstrual pain may also benefit from hormonal birth control pills, which reduce inflammation and regulate periods’ timing and intensity. On top of these medications, complementary therapies like acupuncture, massage therapy, and heat therapy have been found effective by some people.
However, relying solely on medication does not always work out for everyone. In addition to pharmacological interventions, simple lifestyle modifications can play a significant role in easing endometriosis symptoms. Regular exercise can help release feel-good chemicals called endorphins into your bloodstream while promoting healthy blood flow throughout your body. A diet rich in anti-inflammatory foods such as fruits, vegetables, whole grains, and fish oil supplements along with avoidance of caffeine or alcohol consumption during menstruation may also aid in reducing menstrual-related agony.
In conclusion, dealing with endometriosis requires a multi-pronged approach that includes both medical intervention and self-care practices. Pain management techniques ranging from over-the-counter NSAIDs to complementary therapies like acupuncture should be explored based on individual preferences and budget constraints. Additionally, incorporating simple yet impactful lifestyle changes like regular exercise and dietary modifications can go a long way in keeping endometrial flare-ups at bay.
Lifestyle Changes For Endometriosis
Living with endometriosis can be a challenging experience, but there are lifestyle changes you can make to help manage your symptoms. Juxtaposed against traditional pain management methods, these changes may seem small or insignificant, but they can have a significant impact on your daily life.
One of the most important lifestyle changes for managing endometriosis is maintaining a healthy diet. Eating nutrient-rich foods and avoiding processed or inflammatory foods can reduce inflammation in the body, which can alleviate pain and discomfort. Additionally, regular exercise has been shown to decrease menstrual cramps and improve the overall quality of life for those living with endometriosis.
Another key change is stress reduction. Stress has been linked to increased pain levels in individuals with endometriosis, so finding ways to relax and unwind is crucial. This could include practicing yoga or meditation, taking warm baths, or engaging in hobbies that bring joy and relaxation.
To further emphasize the importance of lifestyle changes for managing endometriosis symptoms, here are five additional tips:
- Get enough sleep each night
- Limit caffeine intake
- Avoid smoking and excessive alcohol consumption
- Use heat therapy (such as heating pads) during painful periods
- Consider alternative therapies such as acupuncture or chiropractic care
By implementing these lifestyle changes into your daily routine, you may find relief from the pain and discomfort associated with endometriosis. However, it’s important to remember that every person’s experience with this condition is unique. It may take some time to figure out what works best for you.
As you begin making positive changes towards better health and wellness with endometriosis in mind, keep in mind that coping mechanisms will also play an essential role in how you live day-to-day while dealing with this condition.
Coping With Endometriosis
It can be incredibly difficult to cope with endometriosis. The chronic pain, fatigue, and emotional toll it takes on a person can be overwhelming. However, there are ways to manage the symptoms and maintain a positive outlook.
Firstly, self-care is essential when coping with endometriosis. This means taking care of yourself physically, mentally, and emotionally. It’s important to prioritize rest as much as possible. Gentle exercises such as yoga or swimming can also help alleviate some of the discomfort associated with endometriosis. Finally, seeking out support groups or therapy can provide an outlet for processing emotions related to your condition.
Secondly, managing stress is crucial in coping with endometriosis. Endometriosis itself can cause stress due to its impact on daily life, but external factors such as work or family responsibilities can compound this stress even further. Finding healthy outlets for stress relief such as meditation or journaling can make a big difference in overall well-being.
Lastly, making necessary accommodations in daily life can also aid in coping with endometriosis. This could mean modifying work hours or duties if needed, communicating openly with loved ones about your limitations and needs, or finding alternative methods of birth control that may better suit your body.
Coping with endometriosis is no easy feat, but prioritizing self-care, managing stress levels, and making accommodations where necessary can greatly improve the quality of life for those affected by this condition. In the next section, we will dive into available resources that offer additional support for those living with endometriosis.
Support And Resources For Endometriosis
Living with endometriosis can be tough, but it doesn’t have to be a battle that you fight alone. There are plenty of resources available for those who need support in dealing with this condition, whether it’s through online communities or local support groups. Here are some options for finding help and connecting with others who understand what you’re going through.
Firstly, if you’re looking for reliable information about endometriosis, the Endometriosis Foundation of America is an excellent resource. They offer educational materials on diagnosis, treatment options, and coping strategies for living with the condition. Additionally, their website includes links to various support groups and advocacy organizations that may be helpful to connect with.
Another option is seeking out social media groups dedicated to endometriosis. These online communities provide a space where people can share experiences and ask questions without fear of judgment. Having access to these supportive networks can make all the difference in managing symptoms and feeling less isolated.
Lastly, don’t underestimate the power of reaching out to friends and family members for emotional support. Sometimes having someone to talk to can alleviate stress levels significantly during difficult times when one needs encouragement the most.
Finding support while navigating life with endometriosis isn’t always easy, but there are many useful resources available today that were not around even five years ago. With a little research and effort invested into building your circle of supporters, whether they come from online forums or offline channels- anyone can find comfort in knowing they’re not alone in this journey towards healing themselves physically AND emotionally.
Frequently Asked Questions
Can Endometriosis Affect Fertility?
Did you know that endometriosis affects up to 10% of women worldwide? This condition occurs when the tissue similar to the lining of your uterus grows outside it, causing pain and discomfort. While many people associate endometriosis with painful periods, bloating, and cramping, there is also a concern about how this condition can affect fertility.
Endometriosis can impact fertility in several ways. First, the abnormal growths could damage or block the fallopian tubes, making it difficult for sperm to reach an egg. Second, inflammation caused by endometrial tissue might interfere with ovulation or implantation of a fertilized egg into the uterus. Thirdly, studies suggest that women with endometriosis may have lower-quality eggs than those without.
However, not all hope is lost if you have endometriosis and want to conceive. Many treatment options are available depending on the severity of your case. Hormonal therapies like birth control pills can help regulate menstrual cycles and reduce symptoms while increasing the chances of pregnancy. Surgery is another option where doctors remove as much of the abnormal tissue as possible.
In conclusion, endometriosis can indeed impact fertility but does not necessarily mean infertility. If you struggle with painful periods and suspect you may have this condition, consult with your doctor about potential treatments before trying to conceive. Remember that modern medicine offers innovative solutions every day.
Is Endometriosis Hereditary?
Endometriosis is a condition that affects 1 in 10 women of reproductive age. It occurs when the tissue that lines the uterus grows outside of it, causing pain, inflammation, and potentially infertility. But what causes this condition? Is endometriosis hereditary?
To answer this question, we need to look at the research. While there is no definitive answer yet, studies suggest that genetics may play a role in endometriosis. According to one study published in Human Reproduction Update, individuals with first-degree relatives (mother or sisters) who have been diagnosed with endometriosis have an increased risk of developing the disease themselves.
However, it’s not just genes that determine whether someone develops endometriosis or not. Environmental factors such as diet and exposure to toxins also seem to be involved. This means that even if you don’t have any family history of endometriosis, you could still develop the condition if you are exposed to certain environmental triggers. In other words, while genetics can increase your risk for endometriosis, they do not necessarily guarantee its development.
Just like how a seed needs both sunlight and water to grow into a plant, our genetic predispositions need external factors to manifest into physical conditions such as endometriosis. So while genetics may provide us with some clues about why some people develop endometriosis over others, it’s important not to overlook other potential contributing factors such as lifestyle choices and environmental exposures. By taking a holistic approach to understanding this complex condition and advocating for more research on its causes and cures, we can empower ourselves and future generations with greater knowledge and control over our health outcomes.
Can Endometriosis Be Cured?
Endometriosis is a condition that affects millions of women worldwide. It occurs when tissue similar to the lining of the uterus grows outside the uterus, causing pain and discomfort during menstruation and intercourse. Women with endometriosis often wonder if there is a cure for this debilitating disease.
Unfortunately, there is no known cure for endometriosis. However, several treatments can help manage symptoms and improve quality of life. These include pain medication, hormone therapy, surgery, and alternative therapies like acupuncture and chiropractic care. While these treatments may not cure endometriosis completely, they can provide relief from pain and other symptoms associated with the condition.
It’s essential to remember that every woman’s experience with endometriosis is unique, so treatment options will vary depending on individual circumstances. Additionally, some women may find that their symptoms disappear altogether after menopause since estrogen levels decrease significantly at this time. Therefore it’s crucial to work closely with your healthcare provider to develop an effective treatment plan that meets your needs while keeping in mind that curing endometriosis entirely may not be possible yet.
In conclusion, while there might not be a definitive cure for endometriosis at present, patients have access to numerous resources aimed at managing its symptoms effectively. The focus should remain on finding ways to mitigate the impact of the condition on one’s quality of life rather than seeking a one-size-fits-all solution. With proper medical attention and care along with support from loved ones or groups dedicated to providing aid in this area, we can all strive towards better management practices for those suffering from this ailment today.
Does Endometriosis Increase The Risk Of Certain Cancers?
As a woman, the thought of developing cancer is already nerve-wracking. But what if you have endometriosis? Does having this condition increase your risk of certain cancers? The answer is not straightforward, but let’s delve deeper into it.
Firstly, it’s important to understand that Endometriosis itself is not cancerous. It occurs when tissue similar to the lining of the uterus grows outside of it and onto other organs or tissues in the body. However, some studies suggest that women with endometriosis may be at higher risk for specific types of ovarian and breast cancers than those without the condition. This heightened risk could be due to several factors such as genetic predisposition, hormonal imbalances, or prolonged inflammation.
It’s crucial to note that even though there might be an increased risk, many women with endometriosis never develop these cancers. Hence regular check-ups with your healthcare provider are necessary to catch any abnormalities early on. In conclusion, while more research needs to be done on this topic, being aware of your family history and getting screened regularly can help detect any potential issues down the line. Remember: knowledge is power.
Can Endometriosis Be Prevented?
Endometriosis is a chronic condition that affects the reproductive system of women. It occurs when the tissue lining inside the uterus grows outside it, leading to pain and discomfort during menstruation. While endometriosis can be managed with medications and surgery, many people wonder if there is any way to prevent this condition from occurring in the first place.
Currently, there is no known way to prevent endometriosis entirely. However, researchers have identified some factors that may increase your risk of developing this condition. For instance, genetics play a role in determining whether or not you may get endometriosis; having a family member with endometriosis increases your chances of getting it as well. Additionally, certain lifestyle choices such as smoking or exposure to environmental toxins may also contribute to its development.
Despite these findings, there are still ways for individuals to manage their risk of developing endometriosis. Maintaining a healthy weight through regular exercise and eating a balanced diet can help regulate hormones that affect menstrual cycles and reduce inflammation throughout the body. Avoiding exposure to harmful chemicals found in pesticides and other industrial products may also lower one’s risk of developing this condition.
In summary, while we cannot eliminate our risk of developing endometriosis, taking steps towards living a healthy lifestyle can significantly improve our overall health outcomes and possibly reduce our likelihood of experiencing this painful condition. By staying informed about potential risk factors and making conscious decisions about our daily habits and environment, we can work towards preventing illnesses like endometriosis from negatively impacting our lives.
Conclusion
In conclusion, Endometriosis is a condition that can cause severe pain and discomfort for those who suffer from it. It’s important to understand the causes of endometriosis so that we can better diagnose and treat this condition. The diagnosis process includes several tests, such as pelvic exams, ultrasounds, and laparoscopies.
There are four stages of endometriosis – minimal, mild, moderate, and severe – with each stage requiring different treatment options. Treatment may include medication or surgery depending on the severity of the symptoms. Pain management is also an essential part of treating endometriosis, with options ranging from over-the-counter pain relievers to prescription medications and heat therapy.
To manage endometriosis effectively, lifestyle changes are often recommended. These changes might include adopting a healthy diet rich in fruits and vegetables while avoiding processed foods and sugar-laden drinks; getting regular exercise; managing stress levels through mindfulness practices like meditation or yoga; and limiting alcohol consumption.
Overall, seeking help early on is crucial when dealing with endometriosis. Proper diagnosis and treatment plans in place along with making necessary lifestyle adjustments using the available resources provided by healthcare professionals will allow individuals living with this chronic disease live to their lives comfortably without being held back by its limitations.
Also Read
Recognizing the Unusual Symptoms of Inflammatory Breast Cancer